Recommendations for treatment of HF in patients with HFrEF and diabetes:
- Sodium–glucose co-transporter-2 (SGLT2) inhibitors (dapagliflozin, empagliflozin, or sotagliflozin) are recommended in all patients with HFrEF and T2DM to reduce the risk of HF hospitalization and CV death.
- Sacubitril/valsartan or an angiotensin-converting enzyme inhibitor (ACE-I) is recommended in all patients with HFrEF and diabetes to reduce the risk of HF hospitalization and death.
- Beta-blockers are recommended in patients with HFrEF and diabetes to reduce the risk of HF hospitalization and death.
- Mineralocorticoid receptor antagonists (MRAs) are recommended in patients with HFrEF and diabetes to reduce the risk of HF hospitalization and death.
- An intensive strategy of early initiation of evidence-based treatment (SGLT2 inhibitors, angiotensin receptor–neprilysin inhibitor (ARNI)/ACE-Is, beta-blockers, and MRAs), with rapid up-titration to trial-defined target doses starting before discharge and with frequent follow-up visits in the first 6 weeks following a HF hospitalization is recommended to reduce re-admissions or mortality.


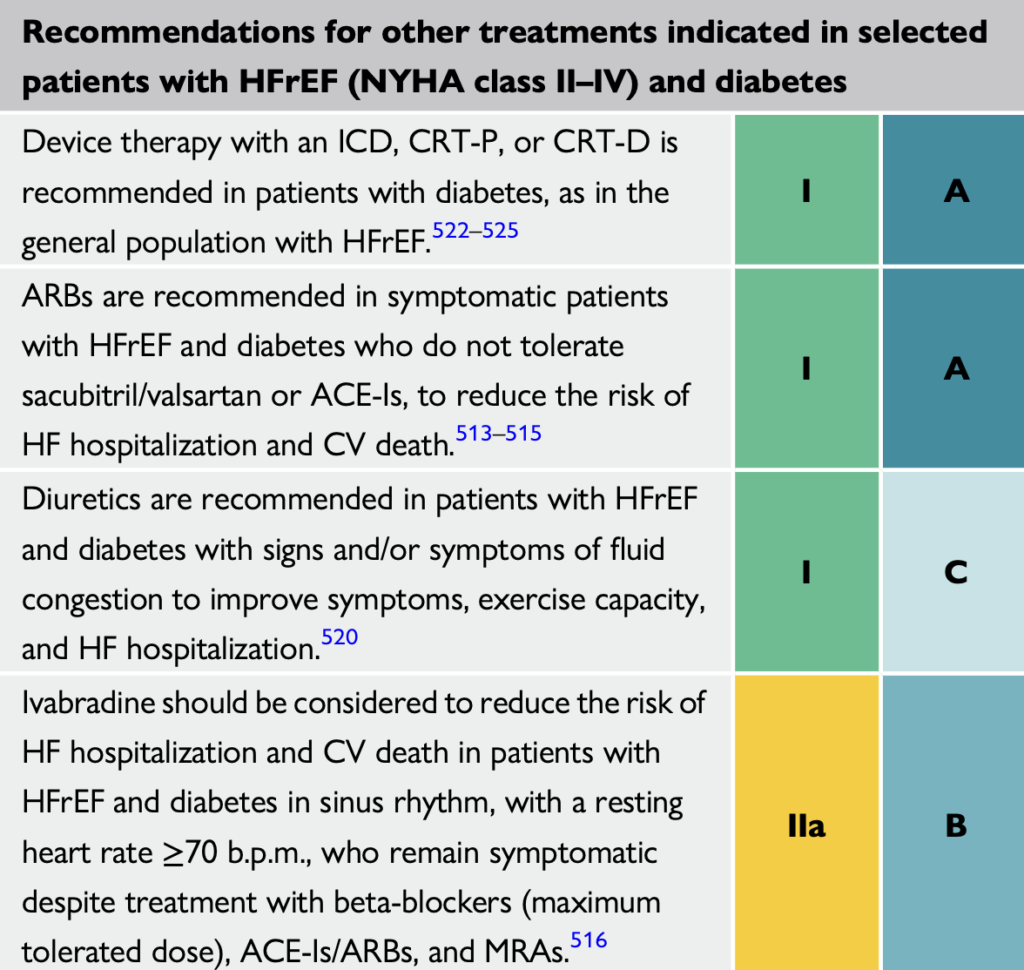
Recommendations for other treatments indicated in select patients with HFrEF (NYHA class II-IV) and diabetes:
- Device therapy with an implantable cardioverter-defibrillator (ICD), cardiac resynchronization therapy-pacemaker (CRT-P), or CRT wit an implantable defibrillator (CRT-D) is recommended in patients with diabetes, as in the general population with HFrEF.
- ARBs are recommended in symptomatic patients with HFrEF and diabetes who do not tolerate sacubitril/valsartan or ACE-Is, to reduce the risk of HF hospitalization and CV death.
- Diuretics are recommended in patients with HFrEF, HFmrEF, and HFpEF and diabetes with signs and/or symptoms of fluid congestion to improve symptoms, exercise capacity, and reduce HF hospitalization.
- Ivabradine should be considered to reduce the risk of HF hospitalization and CV death in patients with HFrEF and diabetes in sinus rhythm, with a resting heart rate ≥70 bpm, who remain symptomatic despite treatment with beta-blockers (maximum tolerated dose), ACE-Is/ARBs, and MRAs.
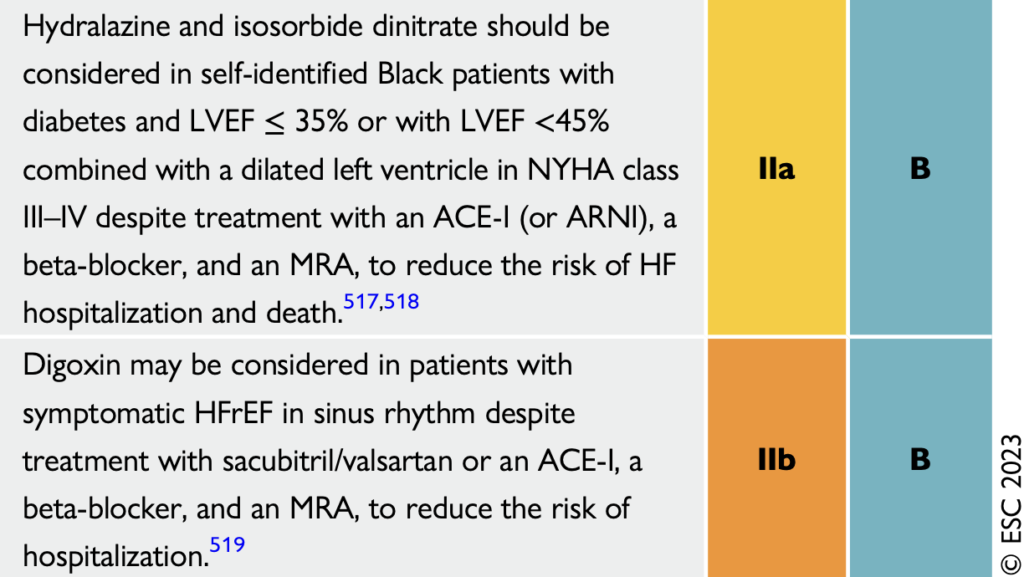
- Hydralazine and isosorbide dinitrate should be considered in self-identified Black patients with diabetes and LVEF ≤35% or with LVEF <45% combined with a dilated left ventricle in NYHA class II–IV despite treatment with an ACE-I (or ARNI), a beta-blocker, and an MRA, to reduce the risk of HF hospitalization and death.
- Digoxin may be considered in patients with symptomatic HFrEF in sinus rhythm despite treatment with sacubitril/valsartan or an ACE-I, a beta-blocker, and an MRA, to reduce the risk of hospitalization.
Recommendations for glucose-lowering medication in patients with T2DM with and without heart failure:
- SGLT2 inhibitors empagliflozin, canagliflozin, dapagliflozin, ertugliflozin, or sotagliflozin are recommended in patients with T2DM with multiple atherosclerotic CVD (ASCVD) risk factors or established ASCVD to reduce the risk of HF hospitalization.
- SGLT2 inhibitors epagliflozin or dapagliflozin are recommended in patients with T2DM and LVEF >40% (HFmrEF and HFpEF) to reduce the risk of HF hospitalization or CV death.
- SGLT2 inhibitors dapagliflozin, empagliflozin, or sotagliflozin are recommended in patients with T2DM and HFrEF to reduce the risk of HF hospitalization and CV death.
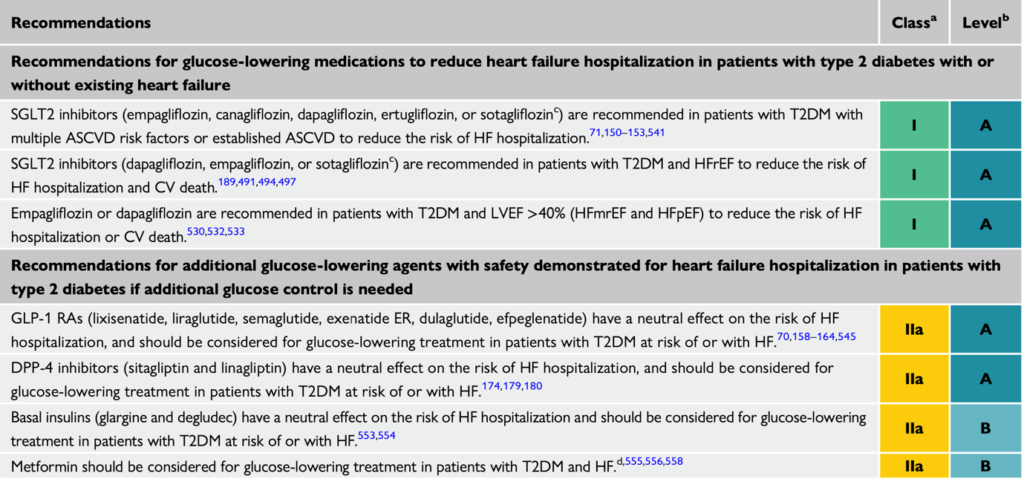
Recommendations for additional glucose-lowering agents with safety demonstrated for HF hospitalization in patients with T2DM if additional glucose control is needed:
- Metformin should be considered for glucose-lowering treatment in patients with T2DM and HF.
- Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) (liraglutide, semaglutide, exenatide extended release, dulaglutide) have a neutral effect on the risk of HF hospitalization, and should be considered for glucose-lowering treatment in patients with T2DM at risk of or with HF.
- Dipeptidyl peptidase-4 (DPP-4) inhibitors (sitagliptin and linagliptin) have a neutral effect on the risk of HF hospitalization, and should be considered for glucose-lowering treatment in patients with T2DM at risk of or with HF.
- Basal insulins (glargine and degludec) have a neutral effect on the risk of HF hospitalization and should be considered for glucose-lowering treatment in patients with T2DM at risk of or with HF.
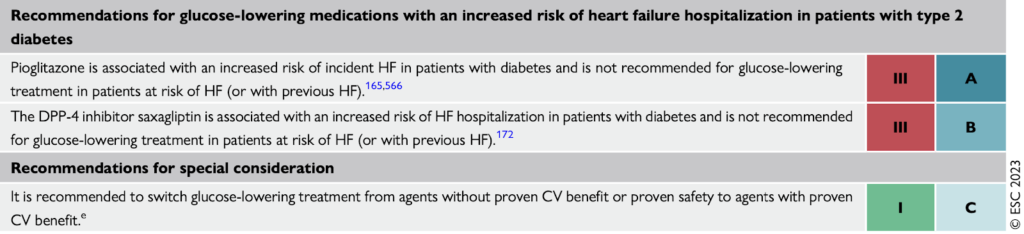
Glucose-lowering medications with an increased risk of HF hospitalization in patients with diabetes:
- Pioglitazone is associated with an increased risk of incident HF in patients with diabetes and is not recommended for glucose-lowering treatment in patients at risk of HF (or with previous HF).
- The DPP-4 inhibitor saxagliptin is associated with an increased risk of HF hospitalization in patients with diabetes and is not recommended for glucose-lowering treatment in patients at risk of HF (or with previous HF).

